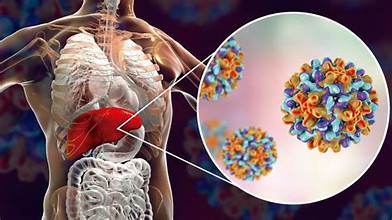
Hepatitis B is a contagious viral infection that primarily targets the liver, causing inflammation and damage. Hepatitis B is a liver infection caused by the hepatitis B virus (HBV), which can be prevented through vaccination. The virus spreads when blood, semen, or other body fluids from an infected person enter the body of someone who is not infected.
The illness may present as a mild, short-term (acute) infection that lasts only a few weeks, or it can develop into a serious, long-term (chronic) condition that requires ongoing medical care.
Types of Hepatitis B:
There are two main types of hepatitis b depending upon how long the virus is present in your body.
Acute Hepatitis B:
Acute hepatitis B is a temporary infection that develops within the first six months after a person is exposed to the hepatitis B virus (HBV). In many cases, individuals may not notice any symptoms, while others may experience only mild signs of illness. However, for some, the infection can become more intense and may require hospitalization due to complications.
Typical symptoms can include fatigue, fever, nausea, abdominal pain, dark urine, and yellowing of the skin or eyes (jaundice). Although most people with acute hepatitis B recover fully and develop lifelong immunity, a small percentage may progress to chronic infection, especially if their immune system cannot completely clear the virus.
Key Insights on Acute Hepatitis B:
- Nearly half (48%) of reported acute hepatitis B infections occurred among individuals aged 40 to 59 years.
- The overall number of newly reported acute cases remained fairly stable throughout 2023, showing no major increase or decline.
- Infection rates were highest among non-Hispanic Black populations, highlighting ongoing disparities in disease burden.
- Geographically, the Appalachian region and nearby states recorded the greatest concentration of acute hepatitis B cases.
Chronic Hepatitis B:
When acute hepatitis B does not clear from the body, it can progress into a long-lasting condition called chronic hepatitis B. Without proper management or treatment, this form of the disease can cause severe complications such as liver damage, cirrhosis (scarring of the liver), liver cancer, and even death.
- People with chronic hepatitis B may live for years without obvious symptoms, which makes regular medical check-ups and monitoring crucial. Although there is currently no cure, antiviral medications can help suppress the virus, protect the liver, and lower the risk of complications. Early diagnosis, lifestyle adjustments, and ongoing medical care greatly improve long-term health outcomes for those living with chronic hepatitis B.
Chronic Hepatitis B in the United States Key Statistics:
- The CDC estimates that nearly 640,000 adults across the U.S. are living with chronic hepatitis B.
- In 2023, non-Hispanic Asian and Pacific Islander (A/PI) populations had the highest prevalence of chronic hepatitis B.
- The rate of newly reported chronic cases among A/PI individuals was almost 10 times greater than that observed in non-Hispanic White populations.
Causes and Transmission of Hepatitis B:
Hepatitis B is transmitted when the blood, saliva, semen, or other bodily fluids of an infected person enter the body of someone who is not infected. A person carrying the hepatitis B virus (HBV) can spread it to others even if they show no signs of illness.
The most common ways the virus is passed from one person to another include:
- Sharing needles, syringes, or other drug-injecting tools.
- Using personal items like toothbrushes, razors, or medical devices (such as glucose monitors) that may have traces of infected blood.
- Having direct contact with the blood or open wounds of someone carrying HBV.
- Engaging in unprotected sexual activity with an infected partner.
- Accidental injuries from contaminated needles or sharp instruments in healthcare or other settings.
- Inadequate infection control in medical or dental facilities.
- Transmission from mother to child during pregnancy, childbirth, or shortly after delivery.
Although HBV can sometimes be detected in saliva, casual activities such as kissing, hugging, sharing food, drinks, or utensils, coughing, sneezing, or breastfeeding do not spread the virus.
Awareness about safe practices, timely vaccination, and strict infection control measures are essential to reduce the risk of transmission. Preventing blood-to-blood contact remains the most effective way to stay protected.
Signs and symptoms:
Many individuals infected with the hepatitis B virus (HBV) may not show any noticeable symptoms. When symptoms do appear during an acute infection, they usually develop around 90 days after exposure. The signs of acute and chronic HBV can look alike, but in most cases, people with chronic infection remain symptom-free for many years. Often, symptoms of chronic hepatitis B only become apparent much later in life, sometimes even decades after the initial infection.
The symptoms of hepatitis B can vary in severity and may affect different parts of the body. Common signs include dark-colored urine or pale, clay-like stools, along with persistent fatigue and fever. Many people also experience joint pain, loss of appetite, nausea, stomach discomfort, or vomiting. In more noticeable cases, the infection can cause jaundice, which appears as a yellowing of the skin and eyes.
Hepatitis B Diagnosis:
Your doctor will do a physical exam and ask about your:
- Symptoms
- Health history
- Family history of liver disease
- Other things that might increase your risk of getting viral hepatitis
But the only way to know if you have hepatitis B is to do blood tests and other tests to check for liver damage and other liver diseases.
Hepatitis tests:
The CDC recommends testing with a triple panel test that includes:
Hepatitis B surface antigen (HBsAg): Antigens are proteins on the surface of HBV that your immune system recognizes as a foreign invader. If you have HBsAg in your blood, it shows you have been infected with HBV and can infect other people.
Hepatitis B surface antibody (anti-HBs): Antibodies are proteins your immune system makes to fight HBV. If you have anti-HBs in your blood, it shows that you have fought off HBV and now can’t get it. Or this can show that you have gotten the hepatitis B vaccine.
Total antibody to hepatitis B core antigen (anti-HBs): This tests for a couple of kinds of antibodies your immune system makes to fight off HBV. If you have anti-HBs in your blood, it shows that you have an ongoing infection or a previous infection with HBV, but your body won’t make this if you’ve gotten the hepatitis B vaccine.
Another blood test you doctor may order is the IgM antibody to hepatitis core antigen (IgM anti-HBs) test. If you have IgM anti-HBs in your blood, then you were infected with HBV less than 6 months ago, so you likely have acute hepatitis B.
If you are pregnant, you should also have a blood test for HBV DNA to see if you need to take antiviral medicine to prevent passing on HBV to your baby.
After you’re diagnosed with hepatitis B, your doctor may order blood and imaging tests (such as an ultrasound) to check if your liver has been damaged by HBV. You may also get regular (about every 6 months) checkups and testing for liver disease.
Treatment of Hepatitis B:
Prophylactic Treatment
Prophylactic treatment refers to preventive care, where medications are given to reduce the chance of developing a disease after exposure. In the case of hepatitis B, this approach is most effective when started within 24 hours of contact with the virus. Common preventive measures include:
- Hepatitis B vaccination: A series of vaccine doses that train the immune system to recognize and fight the virus.
- Hepatitis B immune globulin (HBIG): A preparation of antibodies that provides immediate, short-term protection against HBV.
Treatment for Acute Hepatitis B:
There is no specific antiviral therapy for acute hepatitis B. Most people recover with supportive care. If symptoms such as vomiting or diarrhea are severe, healthcare providers may give intravenous (IV) fluids to prevent dehydration, which happens when the body loses too much fluid to function properly. Rest, hydration, and monitoring are the main strategies until the infection clears naturally.
Treatment for Chronic Hepatitis B:
Management of chronic hepatitis B depends on a person’s overall health, symptoms, and stage of infection. Options include:
- Regular monitoring (surveillance): Routine checkups every 3–6 months, with blood work and imaging tests, to track liver function and detect complications such as cirrhosis or cancer early.
- Medication: Long-term antiviral drugs or immune-based therapies can help control the virus, lower liver damage, and reduce the risk of transmission. In most cases, these medicines are taken for life.
- Surgical options: If hepatitis B leads to liver cancer, surgery may be needed to remove the affected portion of the liver. In advanced cases of liver failure or widespread cancer, a liver transplant may be necessary.
Prevention of Hepatitis B:
Ways to Protect Yourself from Hepatitis B:
The most effective protection against hepatitis B is vaccination, which is given in a series of three doses over six months to ensure full immunity. While waiting for complete protection, there are several steps you can take to lower your risk of infection:
- Use protection during sexual activity: Always practice safe sex, especially if you are unsure of your partner’s hepatitis B status. Latex or polyurethane condoms can significantly reduce the risk.
- Avoid sharing personal items: Items like razors, toothbrushes, or nail clippers can carry traces of infected blood and should never be shared.
- Be cautious with needles: If you use intravenous drugs, do not share syringes or needles. Safe needle practices are critical to preventing HBV transmission.
Maintaining good hygiene and following safe health practices further strengthen your protection until the vaccine offers full immunity.
How to Avoid Spreading Hepatitis B to Others?
The most important step in preventing transmission is to know your status. The CDC recommends that all adults aged 18 and older be screened for hepatitis B at least once.
If you are diagnosed with acute hepatitis B, it’s best to limit close contact with others and stay home from work or social activities until your symptoms have resolved, as this is when the infection is most contagious. For those with chronic hepatitis B, healthcare providers may prescribe antiviral medications to lower the amount of virus in your blood, which significantly reduces the chance of passing it on to others.
In addition, practicing safe sex, avoiding the sharing of personal items or needles, and ensuring household contacts are vaccinated are key steps in protecting loved ones and the community.
Conclusion:
Hepatitis B is a serious yet preventable viral infection that primarily affects the liver. It can appear as either an acute, short-term illness or progress into chronic disease with potentially life-threatening complications, including cirrhosis, liver cancer, and liver failure. Despite its risks, hepatitis B is both detectable and manageable with timely diagnosis, regular monitoring, and appropriate treatment.
The most effective defense is vaccination, which provides long-term protection. Preventive measures such as practicing safe sex, avoiding the sharing of personal items or needles, and ensuring proper infection control in healthcare settings—further reduce the risk of transmission. For those already infected, ongoing medical care, antiviral therapy, and healthy lifestyle adjustments can significantly improve outcomes and reduce the spread to others.