What is Alzheimer’s Disease?
Alzheimer’s disease is the leading cause of dementia. It begins when abnormal proteins known as amyloid plaques and neurofibrillary tangles build up in the brain, damaging and eventually killing brain cells. As these cells die, the brain gradually shrinks.
In the United States, approximately 6.9 million people aged 65 and older are living with Alzheimer’s disease, with more than 70% of them aged 75 and above. Globally, out of over 55 million individuals affected by dementia, an estimated 60% to 70% have Alzheimer’s disease.
The early signs of Alzheimer’s often include difficulty remembering recent events or conversations. As the disease progresses, it leads to severe memory loss and impairs a person’s ability to perform daily activities.
While there is currently no cure for Alzheimer’s, its advanced stages can lead to complications such as dehydration, malnutrition, and infections due to loss of brain function. These complications can ultimately be life-threatening.
Alzheimer’s disease was named after Dr. Alois Alzheimer, who first identified it in 1906. He observed unusual changes in the brain of a woman who had suffered from memory loss, speech difficulties, and unpredictable behavior. Upon examining her brain after death, he discovered abnormal clumps now known as amyloid plaques and twisted strands of fibers, referred to as neurofibrillary or tau tangles.
These plaques and tangles remain key hallmarks of Alzheimer’s disease today. Another major characteristic is the breakdown of connections between neurons the nerve cells responsible for sending signals within the brain and between the brain and the rest of the body, including the muscles and organs.
Alzheimer’s disease is the most common cause of dementia in older adults and currently ranks as the seventh leading cause of death in the United States.
What Causes Alzheimer’s Disease?
The exact cause of Alzheimer’s disease is still not completely understood. However, it is believed to result from a combination of several factors, including:
- Age-related brain changes: As people grow older, the brain may undergo changes such as shrinkage, inflammation, damage to blood vessels, and reduced cellular energy production. These changes can harm neurons and disrupt communication between brain cells.
- Genetic factors: Certain genetic variations may increase the risk of developing Alzheimer’s. Both early-onset Alzheimer’s, which appears between ages 30 and 60, and the more common late-onset form, which occurs after age 65, can be influenced by inherited genes. Individuals with Down syndrome are also at higher risk and may develop symptoms as early as their 40s.
- Health, environmental, and lifestyle influences: Conditions such as heart disease, stroke, high blood pressure, diabetes, and obesity as well as exposure to environmental toxins can contribute to the development of Alzheimer’s or accelerate its progression.
Symptoms of Alzheimer’s Disease:
The primary symptom of Alzheimer’s disease is memory loss. In the early stages, individuals may find it difficult to remember recent events or conversations. As the condition progresses, memory problems worsen and other cognitive and behavioral symptoms begin to appear.
At first, a person may recognize their own difficulties with memory or thinking, but over time, these issues become more noticeable to family members or close friends. The brain changes caused by Alzheimer’s lead to symptoms that gradually intensify.
Memory:
While occasional forgetfulness is normal, the memory loss linked to Alzheimer’s is persistent and increasingly disruptive. It can affect a person’s ability to function both at home and at work. Individuals may:
- Repeat the same questions or statements multiple times.
- Forget conversations, appointments, or events.
- Misplace objects in unusual locations.
- Become disoriented in familiar places.
- Forget names of family members or common items.
- Struggle to find the right words or express their thoughts.
Thinking and Reasoning:
Alzheimer’s impairs concentration, logical thinking, and problem-solving skills. Tasks involving numbers such as balancing a checkbook or paying bills become difficult. Multitasking grows nearly impossible, and eventually, a person may lose the ability to recognize or use numbers.
Judgment and Decision-Making:
The disease affects judgment and the ability to make sound decisions. Individuals may dress inappropriately for the weather, make unwise choices in social situations, or struggle to respond to everyday challenges such as handling a kitchen mishap or making safe decisions while driving.
Planning and Performing Familiar Tasks:
Activities that require multiple steps like cooking, organizing, or playing a favorite game become increasingly challenging. In later stages, people may forget how to perform basic tasks such as dressing, grooming, or bathing.
Changes in Personality and Behavior:
Alzheimer’s can also alter mood, personality, and behavior. Common changes include:
- Depression and apathy
- Loss of interest in hobbies or social activities
- Withdrawal from others
- Sudden mood shifts
- Distrust or suspicion
- Aggression or irritability
- Sleep disturbances
- Wandering or restlessness
- Loss of inhibitions
- False beliefs (such as thinking items were stolen)
Preserved Skills:
Even as the disease advances, some abilities often remain intact for longer periods. These preserved skills may include reading, storytelling, singing, listening to music, dancing, drawing, or doing crafts. Such abilities are maintained because they are controlled by areas of the brain affected later in the course of the disease.
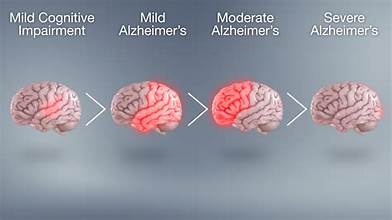
Stages of Alzheimer’s Disease:
Alzheimer’s disease is a progressive condition, meaning it gradually worsens over time. The rate of decline varies for each individual some people experience a slow progression, while others decline more rapidly. Although symptoms may temporarily stabilize, the overall loss of cognitive and physical abilities continues as the disease advances. Alzheimer’s is generally divided into three main stages: early, middle, and late.
1. Early Stage (Mild Alzheimer’s Disease):
In the early stage, a person may begin to notice subtle memory lapses and mild confusion. These changes might seem like normal aging at first, but they gradually become more noticeable. Common signs include forgetting recent conversations or appointments, losing track of time, and misplacing objects.
People in this stage often:
- Have difficulty recalling names or finding the right words.
- Struggle with organizing or managing finances.
- Show decreased ability to plan or make decisions.
- Experience mild mood or personality changes, such as irritability or anxiety.
Despite these challenges, many individuals can still live independently with some support. This is often the stage when Alzheimer’s is first diagnosed, as symptoms become more apparent to family members and friends.
2. Middle Stage (Moderate Alzheimer’s Disease):
The middle stage is usually the longest and most challenging phase for both the person and their caregivers. Damage spreads to brain areas that control language, reasoning, and sensory processing, leading to increased confusion and disorientation.
During this stage, individuals may:
- Have difficulty recognizing familiar faces, including close family members.
- Forget personal history or important life events.
- Wander or get lost in familiar places.
- Struggle with basic tasks such as dressing, bathing, or preparing meals.
- Exhibit personality or behavioral changes, such as agitation, suspicion, or depression.
- Develop disrupted sleep patterns or begin to repeat words and actions.
Daily activities require greater assistance, and supervision becomes necessary to ensure safety. Emotional support and structured routines can help reduce stress and confusion.
3. Late Stage (Severe Alzheimer’s Disease):
In the final stage, Alzheimer’s severely affects all areas of functioning. The brain loses its ability to control basic bodily functions, and individuals become fully dependent on caregivers for their needs.
At this stage, a person may:
- Lose the ability to speak or communicate effectively.
- No longer recognize loved ones.
- Have difficulty swallowing and eating.
- Lose control of movement, balance, and bladder function.
- Spend most or all of their time in bed as the body gradually shuts down.
Comprehensive care is essential in this phase, focusing on comfort, dignity, and quality of life. Families and caregivers often work closely with healthcare professionals to manage symptoms, prevent infections, and ensure the person remains as comfortable as possible.
While the progression of Alzheimer’s disease varies from person to person, early diagnosis, proper medical care, and supportive interventions can help maintain independence and improve quality of life for as long as possible.
How Alzheimer’s Disease Is Diagnosed and Treated?
To diagnose Alzheimer’s disease, doctors typically begin by reviewing a person’s medical history, asking questions about their overall health, and performing cognitive and physical examinations. If Alzheimer’s is suspected, the individual may be referred to a specialist such as a neurologist for a more detailed evaluation.
Specialists can perform additional tests to check for biomarkers, which are measurable signs of disease processes in the body. These biomarkers, found in the brain, blood, or spinal fluid, help determine whether someone has Alzheimer’s or is at risk of developing it. Biomarker testing plays an increasingly important role in diagnosing Alzheimer’s and distinguishing it from other forms of dementia.
Although there is no known cure for Alzheimer’s disease, several medications approved by the U.S. Food and Drug Administration (FDA) can help reduce symptoms or slow their progression. These treatments are often combined with lifestyle and behavioral strategies to help manage daily challenges and improve quality of life.
Most medications are most effective during the early to middle stages of the disease. Meanwhile, researchers continue to study new drug therapies and non-drug approaches aimed at slowing, preventing, or treating Alzheimer’s by targeting its underlying biological causes.
How Alzheimer’s Disease Impacts the Brain?
Alzheimer’s disease causes progressive and irreversible damage to the brain, affecting how a person thinks, remembers, and functions. Long before symptoms become noticeable sometimes 10 years or more before diagnosis subtle and harmful changes begin to take place within the brain.
During these early stages, abnormal proteins start to accumulate, forming sticky clumps called amyloid plaques and twisted fibers known as tau tangles. These protein buildups interfere with communication between nerve cells (neurons) and disrupt normal brain processes. As a result, healthy neurons begin to lose connections with one another, stop functioning properly, and eventually die.
The first areas of the brain typically affected are the hippocampus and entorhinal cortex, regions responsible for memory formation and learning. This is why early symptoms of Alzheimer’s often include forgetfulness and confusion. As the disease advances, the damage spreads to other brain regions involved in language, reasoning, and behavior, leading to worsening cognitive and physical decline.
Over time, the brain’s structure and size change dramatically. The cerebral cortex, which manages thinking and decision-making, thins out, and the spaces within the brain (ventricles) enlarge. By the late stages of Alzheimer’s, widespread neuron loss causes significant brain shrinkage, impairing essential functions like speech, movement, and basic bodily control.
Scientists are still studying the many biological processes involved in Alzheimer’s, including inflammation, vascular damage, and metabolic dysfunction within brain cells. Understanding these changes is crucial for developing treatments that can slow, prevent, or one day stop the progression of this devastating disease.
Prevention and Risk Reduction for Alzheimer’s Disease:
Currently, there is no known way to completely prevent Alzheimer’s disease, but growing research shows that certain lifestyle habits can help lower the risk or delay its onset. Many of these preventive measures are linked to maintaining a healthy heart and brain, as the same factors that protect your cardiovascular system also benefit your brain.
1. Stay Physically Active:
Regular physical activity helps improve blood flow to the brain and supports the growth of new brain cells. Aim for at least 150 minutes of moderate exercise per week, such as walking, swimming, or cycling. Incorporating balance and strength training can also help prevent falls and promote overall brain health.
2. Follow a Brain-Healthy Diet:
A diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats similar to the Mediterranean or DASH diet has been shown to support brain function. These diets emphasize foods high in antioxidants and omega-3 fatty acids that protect brain cells from damage. Limiting saturated fats, processed foods, and refined sugars can further reduce risk.
3. Manage Chronic Conditions:
Health problems like high blood pressure, diabetes, and high cholesterol are linked to an increased risk of cognitive decline. Work closely with your healthcare provider to manage these conditions effectively. Maintaining healthy levels of LDL (“bad”) cholesterol and blood sugar is especially important for protecting both the heart and brain.
4. Quit Smoking and Limit Alcohol:
Smoking damages blood vessels, reducing blood flow to the brain and increasing the buildup of harmful substances. Quitting smoking can significantly reduce dementia risk. Moderate alcohol consumption if any should be practiced, as heavy drinking has been associated with faster cognitive decline.
5. Stay Mentally and Socially Engaged:
Keeping your mind active through learning new skills, reading, puzzles, or playing musical instruments helps strengthen brain connections. Staying socially active through volunteering, joining clubs, or spending time with loved ones can also lower the risk of cognitive decline by reducing stress and depression.
6. Prioritize Good Sleep:
Quality sleep is essential for brain health. During deep sleep, the brain clears out toxins, including excess amyloid proteins linked to Alzheimer’s. Aim for 7–8 hours of uninterrupted sleep each night, and address sleep disorders like insomnia or sleep apnea promptly.
7. Maintain a Healthy Weight and Manage Stress:
Obesity and chronic stress are both associated with higher Alzheimer’s risk. Practicing stress-reducing techniques such as meditation, yoga, deep breathing, or spending time in nature can help maintain both mental and physical health.
Evidence from Research:
A major long-term study in Finland found that people at risk for dementia who made lifestyle improvements focused on healthy eating, regular exercise, and active social engagement experienced slower cognitive decline compared to those who did not.
While there’s no guaranteed way to prevent Alzheimer’s, adopting a brain-healthy lifestyle early and maintaining it consistently can greatly enhance cognitive resilience and overall quality of life as you age.
Conclusion:
Alzheimer’s disease remains one of the most challenging and complex health conditions of our time, affecting millions of people worldwide. Despite the absence of a cure, continuous advancements in research are deepening our understanding of how the disease develops and progresses. Scientists are uncovering the roles of genetics, lifestyle, and environmental factors bringing us closer to effective treatments and early detection methods.
While we cannot yet stop Alzheimer’s, we can take powerful steps to protect our brain health and delay its onset. Regular exercise, a nutritious diet, mental stimulation, and social engagement all contribute to maintaining cognitive strength. Managing chronic conditions such as diabetes, hypertension, and high cholesterol also plays a vital role in reducing risk.
The journey with Alzheimer’s is difficult, but early diagnosis, compassionate care, and informed lifestyle choices can greatly improve quality of life for both patients and caregivers. As medical science continues to evolve, there is growing hope that future therapies will not only slow the disease but eventually prevent or cure it altogether. Until then, awareness, prevention, and support remain our strongest tools in the fight against Alzheimer’s disease.